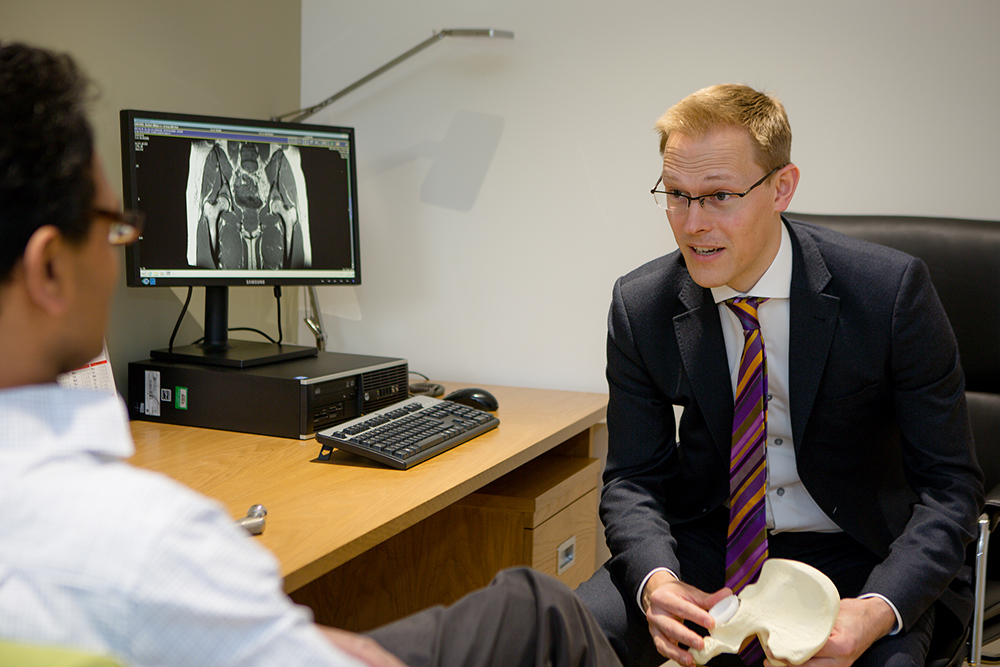
Hip replacement surgery is one of the most successful operative procedures performed on patients worldwide. The vast majority (>95%) of all patients whom have had hip replacement surgery are delighted with the results. There are however a small number of patients who will continue to have pain following total hip replacement surgery or may develop a new pain in a hip replacement which had functioned very well up until that point.
There are a large number potential causes of pain following hip replacement surgery and it is sometimes helpful to think about this in temporal terms :
EARLY (0 – 2 YEARS POST OP)
Normal healing process : the adjustment of soft tissues around the new hip. Most patients heal very well following hip replacement but in some cases it takes a little longer for the soft tissues around the hip to adjust to their new position. Hip joint prostheses can continue to heal for up to a year and sometimes patients can see improvement in function up to 2 years.
Heterotopic ossification : a relatively rare condition where new bone forms in the muscles wround a new hip. This can be painful during the formation stage and lead to stiffness in the longer term.
Infection : Thankfully rare, but can be problematic. An early skin infection may be treated simply with a course of antibiotics but must be seen by your surgeon before this is commenced. Deep infections usually require at least one, but often a series of procedures to clear the infection and restore function. We are exceptionally careful to avoid deep infection occurring at any stage during your patient journey through hip replacement surgery. Occasionally infection may occur as a result of an infection in the blood “seeding” to the hip joint quite unrelated to the hip joint surgery itself.
Fracture : Another rare complication of hip replacement surgery but can occur either during the insertion of a new hip, but is more likely to occur due to a trip or fall.
Iliopsoas impingement : The iliopsoas tendon runs over the front of the hip socket and in some very select cases can be irritated by the new hip socket. There are a number of treatment strategies which may be employed under these circumstances
INTERMEDIATE 2 – 10 YEARS
Early aseptic loosening : With normal use we would expect most modern hip replacements to last at least 15 years. On occasion hip replacements do fail early with no obvious cause. This is most commonly through aseptic loosening, where the implants work their way loose in the absence of infection or another known cause.
Late Infection : This is as above but almost certainly due to seeding of an unrelated infection from the blood (quite commonly from a urinary tract infection). As above this almost certainly requires revision surgery to eradicate the infection.
LATE> 10 YEARS
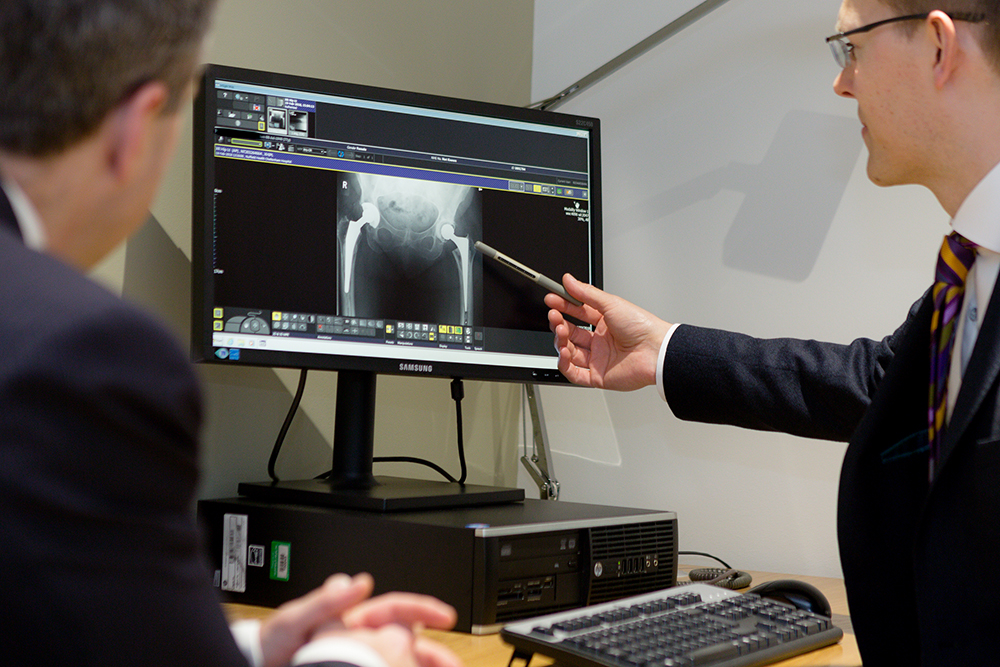
Loose prosthesis : We use the very best bearing combinations and prostheses to reduce the chances of ever requiring revision hip surgery. In common with any device with moving parts eventually hip prostheses will wear out. Overall lifetime risk of requiring hip revision surgery amongst all patients is 5% but we know that younger patients ( <70) will use their hips for longer and often more vigorously which puts this group at higher risk of wearing out their hip and requiring revision (redo) surgery. Patients will usually know when their hip is beginning to wear, but symptoms are classically of ‘startup pain’ just as you rise from a seated position and take the first few steps, and this usually settles to a degree as walking continues. This pain can be in the hip or the thigh, depending on which component is most problematic. If you begin to detect any of these symptoms it’s well worth arranging an xray via your GP to evaluate for a loose prosthesis or alternatively arranging to be seen by a specialist.
Infection following total hip replacement surgery is thankfully very rare but can be very problematic. We breakdown infections into those which are simple post-operative wound infections and those that are deep and involve the hip joint itself.
SUPERFICIAL WOUND INFECTIONS
The good news here is that these usually respond to a course of antibiotics and settle without the need for surgery. On occasion it may be necessary to tidy up the wound with a short operation but this is relatively straight forward with a good outcome. It is important to note that if you do develop a skin infection around your hip wound immediately following surgery you should be reviewed by your surgeon or a member of the team prior to starting antibiotics. Most GPs will ask for the orthopaedic team to see you in A+E in this situation and this allows us to assess the risk to your hip. We may simply start antibiotics but this assessment is important.
PERI-PROSTHETIC INFECTION (INFECTED HIP REPLACEMENT)
Deep infection following total hip replacement surgery is rare but is a difficult problem to deal with. It is treatable but usually requires at least one procedure, or sometimes a series of procedures to change the implants and eradicate the infection. Sadly antibiotics alone are not sufficient to clear infection from the components of the hip replacement. There are several strategies outlined below :
Debridement and implant retention (DAIR)
This technique was pioneered in Oxford and is usually performed for infections that occur acutely and present within 8 weeks within the onset of infection. The hip joint is washed out, infected tissue removed and the ball of the femur and liner of the socket changed to attempt to eradicate the infection. This is then supplemented by a long course of antibiotics. This is the least invasive form of revision for infection with success in 75% of cases.
Single stage revision
Similar to DAIR, but all components are removed and new components implanted within the same sitting. This is also supplemented with a long course of antibiotic therapy with successful eradication of infection in up to 85% of cases.
Two stage revision
The most rigorous form of revision for infection requires removal of all infected tissue and implants and leaves you without a hip until we are confident all infection has been eradicated. At an interval of between 6 and 12 weeks of antibiotic therapy a new hip prosthesis is implanted. This has the best chances of eradication of infection (90%) but is a far bigger procedure to go through in terms of strain on the body.
All of the strategies above have certain indications and are not recommended in all cases. All of our surgical team have expertise in hip revision surgery and will counsel you as to which strategy would suit best.